Clinical Resource: An update on the use of alginate dressings in the diabetic foot
Mandy Yorke, Pam Spruce
The Diabetic Foot Journal Vol 18 No 2 2015
Clinical Resource
AN UPDATE ON THE USE OF ALGINATE DRESSINGS IN THE DIABETIC FOOT
Mandy Yorke, Pam Spruce
The Diabetic Foot Journal Vol 18 No 2 2015
BACKGROUND
Since the introduction of alginate dressings in wound management over 30 years ago (Clarke, 2012), practice has developed and new technologies and dressings have been introduced, with the aim of improving clinical outcomes in the management of diabetic foot ulceration. This article explores the use of alginates in the current management of diabetic foot ulcers and considers the use of a newer product in the alginate dressing range.
BEST PRACTICE AND THE USE OF DRESSINGS
When managing the wound, the principles of wound bed preparation are recommended (European Wound Management Association, 2004) to include effective debridement, the prevention and management of infection, maintaining the moisture balance, which includes prevention of periwound skin maceration, and frequent inspection to observe for changes in the wound, which may necessitate a change of intervention. While dressing products alone will not heal these wounds, they can contribute to an optimal environment to encourage healing and prevent complications, which can lead to deterioration.
There is no ‘ideal dressing’ for diabetic foot ulcers, and as with other wound types there is limited evidence to demonstrate the effectiveness of one product in preference to another. In fact, patients with diabetes are often excluded from clinical research into wound care, unless there is a specific requirement for inclusion. The Cochrane Wounds Group (Dumville et al, 2012) have undertaken a series of reviews into the effectiveness of a number of different wound care products in healing diabetic foot ulcers, one of which is the use of alginate dressings. Only six studies were identified to be relevant and the authors acknowledged that while there was no research evidence to demonstrate the effectiveness of alginate dressings in comparison to other dressings, the trials were small and underpowered and, in most of them, the wounds under investigation were non-complex foot ulcers.
It was suggested in this review that the outcome may be of limited use to clinicians who treat harder-to-heal foot ulcers and they did recommend that decision makers should consider the overall benefits of the dressings, such as exudate management (Dumville et al, 2012). The effective treatment of diabetic foot ulceration is complex, and effective management of the wound bed and periwound skin is important.
ALGINATE DRESSINGS
Within the manufacturing process the soluble sodium alginate is extracted and partially converted to insoluble calcium alginate forming non-woven fibres. Alginate dressings are available as a fibre sheet, rope or ribbon, which becomes a soft gel when in contact with fluid, such as wound exudate. There are different gelling characteristics between alginate dressings where high M alginates have a softer and more elastic gel, which forms quicker than that produced by a G-rich alginate (Clarke, 2012).
Alginate dressings are predominantly used to manage excess exudate. However, it has also been suggested that wound healing may be encouraged by the discharge of calcium ions from the dressing into the wound, caused by the interaction with the sodium ions in the fluid (Thomas, 2000). Although alginate dressings are predominantly used to maintain the moisture balance in the wound, they can also support other interventions.
EXUDATE MANAGEMENT
Effective exudate management is very important in the management of diabetic foot ulcers.
- Chronic wound exudate is considered to contain high levels of inflammatory mediators and activated matrix metalloproteases (World Union of Wound Healing Societies, 2007). If not managed effectively, its presence can impede healing and damage the wound bed and surrounding tissues (Romanelli et al, 2010)
- Excess exudate can impede other recommended interventions. It can cause maceration of the wound margins and periwound skin, which can inhibit effective sharp debridement and subsequently lead to further wound deterioration (Foster, 2006)
- Exudate that has leaked through the dressing can increase the risk of bacterial contamination caused by strikethrough onto the wound from the environment. It can also contaminate and damage any offloading devices, which may need repair or replacement (Speak, 2014)
- Leakage of exudate can be distressing for patients, particularly when it is associated with malodour.
Alginate dressings are recognised as being effective for the absorption and retention of exudate, and it has been suggested that they absorb between 15– 20 times their weight in fluid (Jones, 1999).
SUPPORT WOUND DEBRIDEMENT
This may be removed through maintenance debridement from other techniques, one of which is autolysis. Alginate dressings where there is sufficient exudate to encourage gel formation can facilitate this. Although sharp debridement is beneficial to promote healing, the radical removal of devitalised tissue can frequently result in bleeding, which can be managed through the use of an alginate dressing with haemostatic properties.
FACILITATE GOOD DRESSING TECHNIQUES
Dressing foot wounds can be difficult for clinicians who are inexperienced, and there is the risk that poor application techniques can cause further damage by increasing pressure on ‘at risk’ areas, which may go unnoticed on a neuropathic foot. Alginate dressings are soft and conformable, can be cut to shape around difficult areas, and can be used to pack a cavity wound or to facilitate the drainage of a sinus.
In conjunction with a suitable secondary dressing, they can be used within an offloading device or appropriate footwear without causing additional damage by being too bulky.
ACTIVHEAL AQUAFIBER®
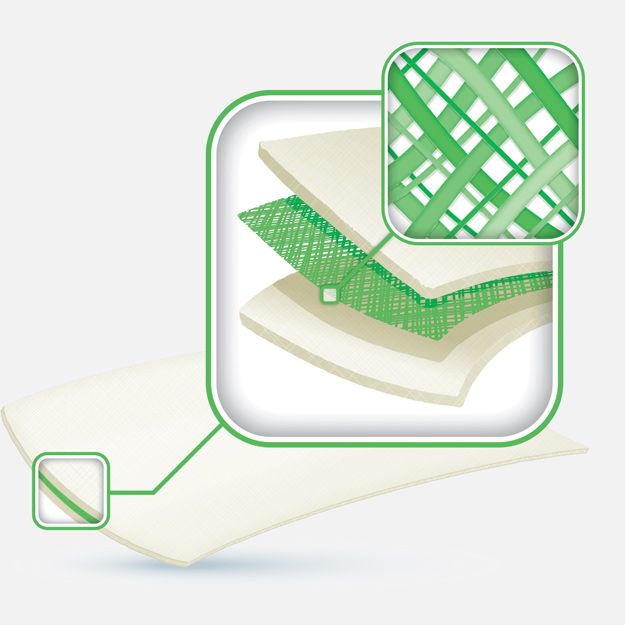
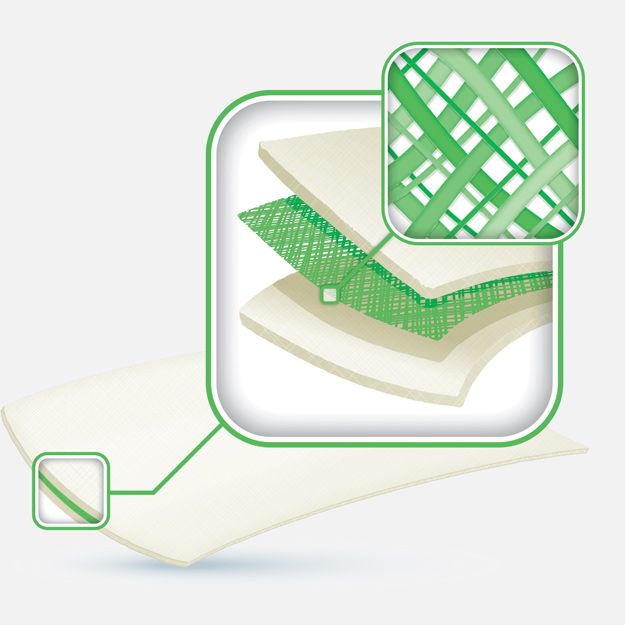
The absorption capacity has been demonstrated in vitro as 23g of fluid per 100 cm2 of dressing over a 24-hour period. When applied to a wound, the dressing fibres come into contact with exudate, and swell to form a soft cohesive gel dressing. This provides intimate contact with the wound bed, and provides an ideal moist environment required to support wound healing.
The dressing is suitable for the management of diabetic foot ulcers as exudate is absorbed and transferred vertically into the dressing, which reduces the risk of maceration and damage to the periwound skin or to the wound itself (Timmons, 2008; Ousey et al, 2011). The high, wet tensile strength allows it be removed intact without leaving any fibres in the wound (Kesteven et al, 2012).
ActivHeal Aquafiber also has haemostatic properties and can be used postsharp debridement to control minor bleeding (Thomas, 2000). As with the majority of alginate products, ActivHeal Aquafiber requires a secondary dressing that should be selected according to the level of exudate, the condition of the periwound skin condition, the capacity within an offloading device (if used) and patient preference.
METHOD: CASE STUDY 1
The wound measured 10mm x 5mm and was 2mm deep, which also undermined the medial lip by 2mm. There was 100% granulation tissue in the wound bed and a high level of exudate, although the periwound skin was dry. The wound required sharp debridement of the wound margins to remove callus and a dressing that would maintain encourage further granulation tissue in the wound bed, as well as provide exudate management.
Following sharp debridement that resulted in some bleeding, the wound was cleansed with an antiseptic solution and ActivHeal Aquafiber was applied to the wound bed. A secondary dressing of sterile gauze was used and the foot offloaded with modified first phase insoles with specific offloading for the wound area in the shoe. Initially, the wound was inspected daily for any signs of deterioration and redressed by the patient’s wife, but as the wound improved after the first week, this was reduced to 3 days.
After 2 weeks, the wound had reduced in size to measure 8mm x 2mm x 1mm depth, with no undermining. As the exudate level was minimal, an alginate dressing was no longer indicated (Figure 1b).
RESULTS

1A. Wound before treatment with the evaluation dressing

1B. Wound at the end of the evaluation period
METHOD: CASE STUDY 2
Although the foot was neuropathic, the patient complained of pain in the wound, which was recorded as level 2 on a visual analogue score where 0 represented no pain and 5 was the worst pain.
The wound measured 16 mm x 18 mm probing to 2 mm deep, with the wound bed assesses as being 10% slough and 90% granulation tissue. There was a moderate level of wound exudate.
A treatment programme of sharp debridement, cleansing with an antiseptic solution and application of ActivHeal Aquafiber to the wound bed was implemented. Sterile gauze and tubular gauze dressings were used as secondary dressings. The foot was offloaded by using first phase insoles with specific offloading for the wound area.
RESULTS

2A. Initial wound assessment

2B. Later wound assessment
CONCLUSION
References
Clarke M (2012) Technology update: rediscovering alginate dressings. Wounds International 3: 24–8
Draget KI, Smidsrød O, Skjåk-Bræk G (2005) Alginates from algae. In: Biopolymers Online. DOI: 10.1002/3527600035. bpol6008
Dumville JC, O’Meara S, Deshpande S, Speak K (2012) Alginate dressings for healing diabetic foot ulcers. Cochrane Database of Systematic Reviews 2. Art. No. CD009110. DOI: 10.1002/14651858.CD009110.pub2
European Wound Management Association (2004) Position document: Wound bed Preparation in Practice. MEP Ltd, London. Available at: http://bit.ly/1J4ecQV (accessed 28.05.2015)
Foster AVM, Greenhill MT, Edmonds ME (1994) Comparing two dressing in the treatment of diabetic foot ulcers. J Wound Care 3: 224–8
Foster AVM (2006) Podiatric Assessment and Management of the Diabetic Foot. Elsevier LTD, London. 225–6
International Best Practice (2013) Best Practice Guidelines: Wound Management in Diabetic Foot Ulcers. Wounds International, London. Available at: http://bit.ly/1M3lf9d (accessed 29.05.2015)
Jones V (1999). Alginate dressings and diabetic foot lesions. The Diabetic Foot Journal 2: 8–14
Kesteven D, Hinde H, Forder R (2012) Performance characteristics of a reinforced high gelling moist wound dressing. Poster Presentation at Wounds UK, Harrogate
Ousey K, Edwards C, Jordan J et al (2011) Case series highlights the clinical effectiveness of the Activheal wound care dressings. MA Healthcare, UK
Romanelli M, Vowden K, Weir D (2010) Exudate Management Made Easy. Wounds International 1: 1–6 Available at: http:// bit.ly/1AoR0pS (accessed 28.05.2015)
Speak K (2014) Management of highly exuding foot ulcers. The Diabetic Foot Journal 17: 64–8
Thomas S (2000a) Alginate dressings in surgery and wound management — Part 1. J Wound Care 9: 56–60
Timmons J (2008) ActivHeal Aquafiber a new soft, conformable highly absorbent dressings for use with chronic wounds. Wounds UK 4: 88–91
World Union of Wound Healing Societies (2007) Principles of Best Practice: Wound Exudate and the Role of Dressings. A Consensus Document. MEP Ltd, London
CONTACT US FOR MORE INFORMATION
Discover ActivHeal®
Social Media
Our Product Range
AMS Group
ActivHeal®, its logo and the Advanced Medical Solutions logos are registered trademarks of Advanced Medical Solutions Ltd.
Copyright © Advanced Medical Solutions Limited | Design by Lumisi Ltd


