Clinical Resource
The implementation of tissue viability link nurse education programme in the mental health setting
Elaine Forster
Tissue Viability Nurse Mental Health/Learning Disabilities
Clinical Resource
The implementation of tissue viability link nurse education programme in the mental health setting
Elaine Forster
Tissue Viability Nurse Mental Health/Learning Disabilities
BACKGROUND
The author has previously outlined the need for a robust link nurse and training programme (Forster 2015), having carried out an audit of mental health nurses knowledge relating to tissue viability and wound care. As a result of the aforementioned, Tissue Viability Link Nurse Education programme was introduced.
Ethical approval was not required as it was an audit of current clinical practice.
METHOD
22 wards including Later Life and Adult Memory (LLAMS), Child and Adolescence MENTAL HEALTH SERVICES (CAMHS), were represented by a nominated Link Nurse. The programme was non discriminatory in regards to pay bands, the criteria being an interest in wound care.
A comprehensive, generic, university approved education programme was chosen (Generic Wound Care Book, ActivHeal, University of Chester), delivered in modular form, over an afternoon once a month for a 6 month period.
Sessions involved workshops, presentations, case studies, discussion forums, with support materials and follow up work books for home learning. Collaboration between Tissue Viability and course facilitator to ensure local protocols were included within the education.
Evaluation and feedback forms were filled in post sessions, allowing the programme to adapt to the needs of the Link Nurses to ensure relevance and engagement was maintained. Wound assessment forms and pressure ulcer referrals were monitored pre and post programme.
RESULTS
The results showed an overall improvement in the level of knowledge with an increase in the awareness of physical factors affecting wound healing. These were, in particular nutrition, pain, medication and other physical diseases.
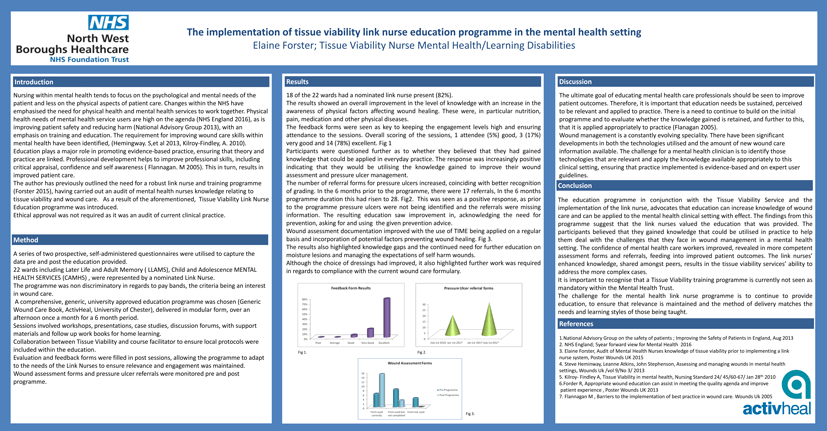
The feedback forms were seen as key to keeping the engagement levels high and ensuring attendance to the sessions. Overall scoring of the sessions, 1 attendee (5%) good, 3 (17%) very good and 14 (78%) excellent.
Fig 1 Participants were questioned further as to whether they believed that they had gained knowledge that could be applied in everyday practice. The response was increasingly positive indicating that they would be utilising the knowledge gained to improve their wound assessment and pressure ulcer management.
The number of referral forms for pressure ulcers increased, coinciding with better recognition of grading. In the 6 months prior to the programme, there were 17 referrals, In the 6 months programme duration this had risen to 28. Fig 2. This was seen as a positive response, as prior to the programme pressure ulcers were not being identified and the referrals were missing information. The resulting education saw improvement in, acknowledging the need for prevention, asking for and using the given prevention advice.
Wound assessment documentation improved with the use of TIME being applied on a regular basis and incorporation of potential factors preventing wound healing. Fig 3.
The results also highlighted knowledge gaps and the continued need for further education on moisture lesions and managing the expectations of self harm wounds.
Although the choice of dressings had improved, it also highlighted further work was required in regards to compliance with the current wound care formulary.
Feedback Form Results (%)
Pressure Ulcer Referral Forms
Wound Assessment Forms
DISCUSSION
Wound management is a constantly evolving speciality. There have been significant developments in both the technologies utilised and the amount of new wound care information available. The challenge for a mental health clinician is to identify those technologies that are relevant and apply the knowledge available appropriately to this clinical setting, ensuring that practice implemented is evidence-based and on expert user guidelines.
CONCLUSION
It is important to recognise that a Tissue Viability training programme is currently not seen as mandatory within the Mental Health Trust.
The challenge for the mental health link nurse programme is to continue to provide education, to ensure that relevance is maintained and the method of delivery matches the needs and learning styles of those being taught.
References
- National Advisory Group on the safety of patients; Improving the Safety of Patients in England, Aug 2013
- NHS England; 5 year forward view for Mental Health 2016
- Elaine Forster, Audit of Mental Health Nurses knowledge of tissue viability prior to implementing a link nurse system, Poster Wounds UK 2015
- Steve Heminway, Leanne Atkins, John Stephenson, Assessing and managing wounds in mental health settings, Wounds Uk /vol 9/No 3/ 2013
- Kilroy- Findley A, Tissue Viability in mental health, Nursing Standard 24/ 45/60-67/ Jan 28th, 2010
- Forder R, Appropriate wound education can assist in meeting the quality agenda and improve patient experience, Poster Wounds UK 2013
- Flannagan M , Barriers to the implementation of best practice in wound care. Wounds Uk 2005
CONTACT US FOR MORE INFORMATION
DISCOVER ACTIVHEAL®

OUR PRODUCT RANGE
AMS GROUP

TRAINING & EDUCATION
Discover ActivHeal®
Our Product Range
AMS Group
Training & Education

ActivHeal is a registered trademark of Advanced Medical Solutions Ltd. Only applicable in the EU.
ActivHeal is a registered trademark of Advanced Medical Solutions Ltd. Only applicable in the EU.
>> Site Map